A few weeks ago, Green made a decision to use the translation equipment provided by El Segundo-based Cloudbreak, an interpretation service which is now providing telemedicine, to help reduce face-to-face visits with patients and in turn save protective gear that might otherwise be used for visits with COVID-19 patients.
Tapping telemedicine is one way doctors, policymakers and administrators like Green hope they can preserve resources and keep staff safe. At least two health care workers in Los Angeles County have died due to the virus and 324 have tested positive. And medical staff around the country are scared as reports of sick nurses and doctors stack up and a shortage of protective equipment persists.
Green and others have begun to deploy technology from smartphones and computers to remote patient monitoring tools in an effort to limit COVID-19 exposure. Meanwhile, jittery patients are flocking to companies that offer remote services rather than risk going into an infected doctor's office. But, telehealth has its limits and doctors can't diagnose everything via a screen.
Cloudbreak's service lets patients talk to doctors from monitors that are carted into their rooms. Like many executives facing the pandemic, the head of Cloudbreak, Jamey Edwards, switched the company's focus as the virus began to ravage the country to one more relevant to the times: telemedicine. Now, demand is booming and he is looking at more services that can help doctors reach patients on their cellphones and beyond. Green has 16 of Cloudbreak's carts in his Los Angeles-based hospitals and ordered another 20 in anticipation of an onslaught of COVID-19 patients.
 Jamey Edwards, CEO of Cloudbreak
Jamey Edwards, CEO of Cloudbreak
It may sound like a small gesture, but the video conference could slow the burn of hospitals' protective equipment by 10% to 15%. Not only is the protective gear more difficult to acquire as demand jumps, but prices are rising just as hospitals and clinics like his are getting squeezed financially as they forgo elective surgeries and other treatments they rely on for revenue.
The standard N95 masks used by doctors previously cost less than $1, but are now being sold for six times the price in some cases.
"This provides another layer of safety to my elderly physician staff as well as just to the rank and file employees," Green said. "They are nervous and rightfully so, because they have never had to unnecessarily risk their own life while treating patients."
At the Gardena hospital, which has a large population of uninsured and nursing home residents, Green said he is looking to use it for COVID-19 patients in the ICU that might normally require consistent monitoring from nurses, saving medical staff from constantly going into check on them.
At Martin Luther King Jr. Community Hospital, Dr. Stanley Frencher who is the medical director of surgical outcomes and quality, says many of these carts will be used in tents outside the hospital to evaluate possible COVID-19 patients, and there will also be one in nearly every room inside the facility. The hospital now has 60 with another 80 on order and a goal of getting to about 160 in the coming weeks.
"You have all these different ways in which telemedicine can be leveraged to ultimately manage this short term need to physically distance ourselves from one another," he said. "In doing so, we will definitely be saving lives by using telemedicine."
Expansion of Telemedicine
To encourage telemedicine use and slow the trajectory of the fast-moving virus, President Donald Trump earlier this month waived restrictions allowing doctors to operate across state lines and relaxed HIPAA compliance allowing doctors to use their own phones to free up hospitals and doctors for COVID-19 patients. This week, the Federal Communication Commission unveiled a $200 million fund to boost telehealth services for hospitals.
Use of remote health services has been surging amid the pandemic.
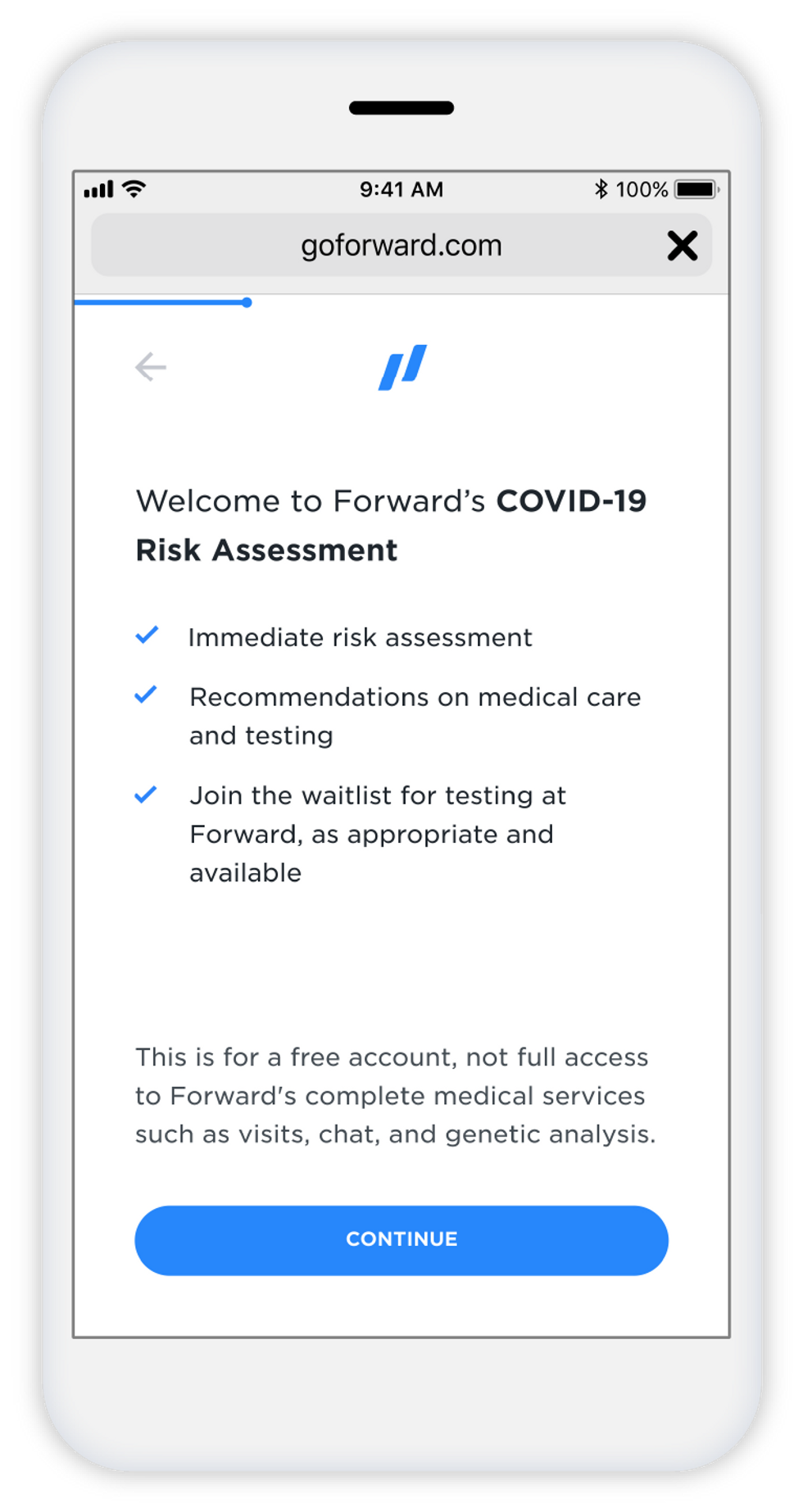
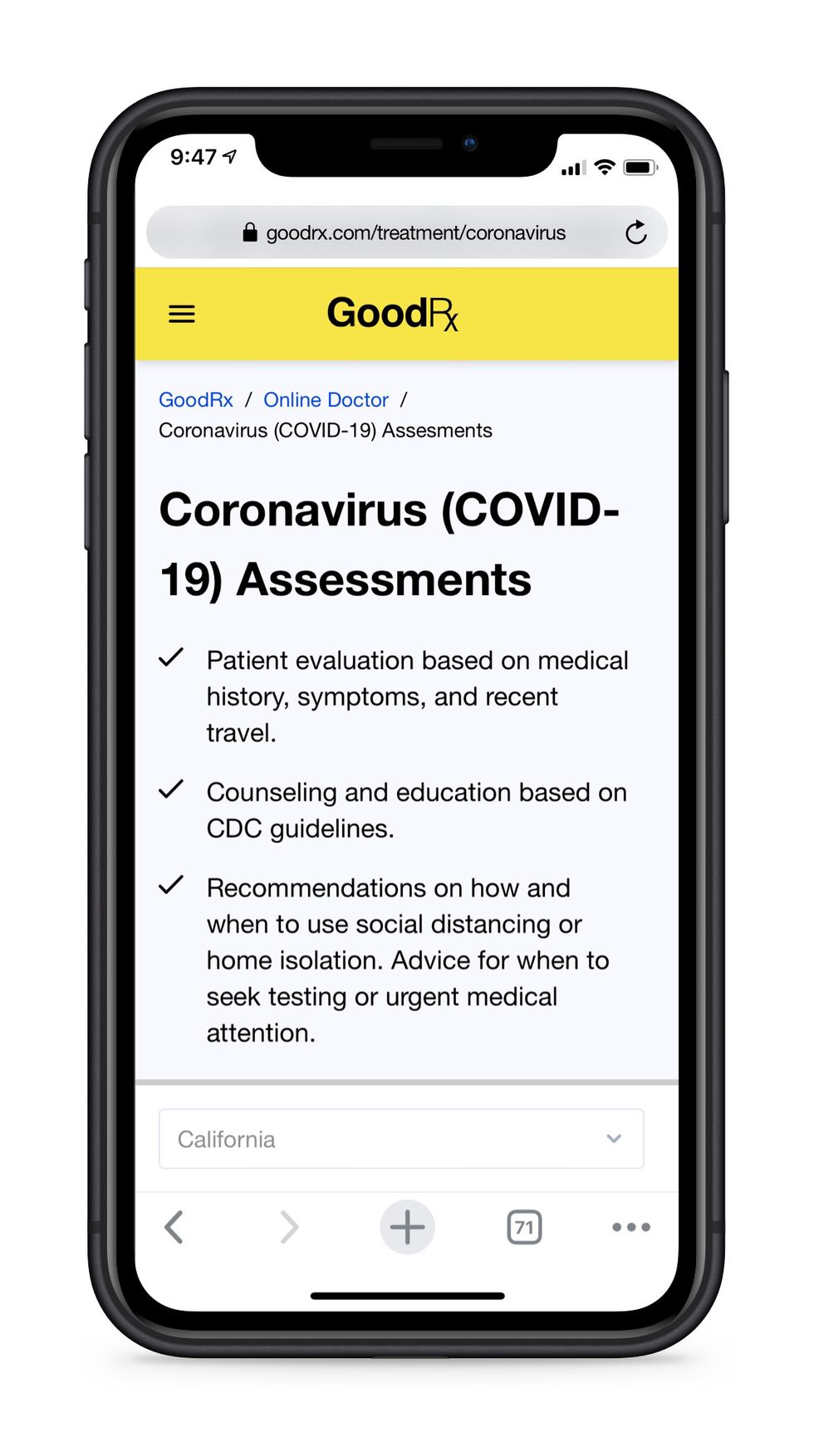
Companies like Los Angeles-based Heal, a primary healthcare service offering home doctor visits from a network of physicians, has seen usage jump 640% over the past month as patients turn online instead of risking going to a doctor's office. The San Francisco-based Forward, a health care subscription service with clinics in Los Angeles, launched a COVID-19 screener. At GoodRx, which acquired HeyDoctor last year, telehealth visits have soared.
"We think this is going to be the new normal for 2020," said John Asalone, who heads telehealth at GoodRx. "People are not going to their primary care doctors right now, but as health issues are still happening (and) they still need their medication, they will either skip care or find it elsewhere."
The $5.6 billion telehealth market in the United States has struggled for years to take off with people reluctant to connect with doctors online, but recently more companies like e-commerce giant Amazon have looked to telehealth to offset the high cost of employee medical coverage. The pandemic has forced people with chronic conditions like diabetes to check in with their doctor online or by phone as clinics and hospitals across the country cancel routine visits and elective surgeries.
"This could almost ironically be the tipping point for telehealth," said Jay Goss, general partner at Pasadena-based venture capital firm Wavemaker Three-Sixty Health that has several telehealth companies in their portfolio. "The core thing these companies do is more valuable today than it was before the pandemic.
"There's a cultural willingness now to do something that for the longest time was just done in person," Goss said.
Limits of Remote Doctors
There's also a dire necessity, but it's an imperfect tool. Doctors can't administer important tests or touch patients. There's technical issues that can pop up. And then, even Cloudbreak's carts that are rolled into ICUs must be sanitized by a human.
Despite this, Alex Fredrick, an analyst at Pitchbook, expects the pandemic will force rapid adoption of telemedicine. He points to companies like InTouch Health, a Santa Barbara company acquired by New York-based Teladoc in January that was used to treat what is believed to be patient zero in Washington.
He expects to see more robots being used to administer services as the sector develops. But that isn't helping people now who cannot be tested remotely.
 The $5.6 billion telehealth market in the United States has struggled for years to take off with people reluctant to connect with doctors online.Photo courtesy of Wikimedia Commons
The $5.6 billion telehealth market in the United States has struggled for years to take off with people reluctant to connect with doctors online.Photo courtesy of Wikimedia Commons
Forward, the subscription health service, tries to bridge some of the gap with their remote tools to monitor patients. But even the clinics in Los Angeles had to set up two drive-thru locations in Glendale and Newport Beach this month in an attempt to prevent carriers of COVID-19 from entering their clinics. And doctors there say there is no substitute for hearing and touching a person up close.
"Sometimes when you are talking to a person over the phone, you think, 'gosh, I really need to listen to this person's lungs. I need to examine them'," said Keith DesRochers, a primary care physician at Forward's clinic in Century City. "People have switched in his world to thinking COVID yes or no 100 percent of the time, but people still get pneumonia, people still get asthma exacerbations, they still get the flu. We need to make sure that we aren't missing those things."
But coming into work is a frightening proposition these days.
"To be honest, primary care doctors aren't used to being fully on the frontlines and putting ourselves at risk," he said. "It's scary, we are all trying to do the best we can to take care of our patients."
***This story was updated April 8 at 1:46 p.m. to reflect the most recent rates of COVID-19 infections and deaths among health care workers as reported by L.A. County health officials.
Reach out to me on Twitter @racheluranga, where my DMs are open, email me at rachel(at)dot.la.
From Your Site Articles
Related Articles Around the Web




 Jamey Edwards, CEO of Cloudbreak
Jamey Edwards, CEO of Cloudbreak